In his book, Sisyphus, Camus describes suicide as an absurd response to fate.
Suicide is a problem. It has been an option to escape emotional suffering for human beings throughout history.
I have treated clients who are suicidal. Preventing suicide is when people are able to work through suicidal thoughts and feelings without acting on them. Tragically, suicide has been the ultimate consequence of the person’s life.
Suicide can happen to anyone, rich and the poor, the well known and the anonymous, professional and working class persons, world leaders. It is a personal act, but it has community and social implications. Suicide tells us something about the people who do it. Robin Williams, the comedian, is an ironic example of a person who you wouldn’t think would kill himself, but he did. There is much speculation around why Robin Williams chose to take his own life, but the truth is we will never know what ultimately compelled him to act as he did.
A SAMPLE OF TELEVISION AND MOVIE PERSONALITIES WHO SUICIDED:
Mya-Lecia Naylor - Actress (Cloud Atlas), suicided April 7, 2019, hanging
Anthony Bourdain, NYT TV personality, food, suicided June 8, 2018, hanging
Stanley Adams, Actor (Breakfast at Tiffany’s) suicided April 27, 1977
Stephanie Adams, Model, suicided May 18, 2018, threw 7 y/o son out 25 story window then jumped.
Clay Adler Actor (Make it or Break it), suicided march 26, 207, gunshot wound to head
Chantal Akerman, Director, suicided October 5, 2015 undisclosed method
Michael Lockwood, Wrestler WWF SmackDown, suicided November 6, 2003, drug overdose
Stan Kirsch, Actor (Highlander), suicided January 11, 2020 hanging
Margo Kidder Actress (Superwoman), suicided May 13, 2018, alcohol overdose
Brian Keith Actor (Parent Trap), suicided June 24, 1997, gunshot wound
Silvio Horta Actor (Ugly Betty), suicided January 7, 2020, gunshot wound to head
Characteristics of a Suicidal Client
I present a set of characteristics from research that differentiates those who will threaten suicide, but not act versus a person who will threaten AND act.
Maladaptive affect (chronically depressed, irritable, aroused, and socially isolated)
Maladaptive cognitions ( expressing hopelessness, negative self-expectations, rigid thinking patterns, and impulsive)
A history of suicidal thinking and throughs
Misuse or a history of misuse of alcohol and other drugs
Substantial Mental Health Diagnoses (Bipolar, Chronic major depression, Anxiety, Schizophrenia, Borderline personality disorder,
A history of major trauma where personal control has been lost (being physically abused as a child, being raped)
The experience of extreme stress from prejudice or discrimination (family rejection, bullying, racial abuse)
Chronic disease or disability (no longer wanting to live because of a terminal cancer diagnosis)
Knowing someone who died by suicide, particularly a close family member
Access to lethal means for killing (having a gun, having lethal pills or drugs, easy access to a bridge from which to jump).
The Case of Craig
Craig was a young married, Caucasian male with no children. For most of his life Craig described himself as not having many psychological issues except that he felt anxious about attending school. He had just completed his college degree and took a job in a sales agency where he was meeting a sales target weekly. At first, he said he enjoyed the work and he was promoted to manager. As time went on, he received feedback that his group was underperforming. His work setting stepped in and tried to educate him, but he began feeling he was unable to perform the job with or without help, and he needed to get out. This led him to conclude he could do nothing right, that he was a deeply flawed human being, that everyone would be better off if he was no longer around. At the same time, Craig’s family began distancing themselves from him because he incessantly talked about his own suicide. His siblings were all successful and he viewed himself as failing to keep up. He felt ashamed when he met with family members at social gatherings, especially his siblings.
As time passed, Craig started having bouts of debilitating anxiety. It was during one of his panic attacks where he described to me laying in bed, sweating and shaking as waves of anxiety rolled through his body back and forth. When these happened he couldn’t think, breathe, move and he felt emotionally and physically paralyzed. He described the waves like rolling pins of electricity. At times, he said he would become so immobilized he occasionally urinated in his bed, unable to get up and walk the few steps to his bathroom.
His wife of one year was fearful of his constant expression of killing himself to escape anxiety. He was eventually hospitalized and when this happened he lost his sales job. During the hospitalization he became immobilized by anxiety several times in the presence of professional staff. It was from this that the decision for Electoconvulsive Therapy (ECT) was made to help break down his supposed anxious thought patterns. I saw him after he was discharged from a second one-week hospital stay. He was taking multiple drugs for bipolar disorder, depression, and anxiety with little effect. He was being followed daily by his psychiatrist, I was seeing him twice weekly, and he was in touch with the ECT staff follow-up team.
In each session, his affect was flat, his forehead was sweating during our first meeting. It took six sessions before he would even talk to me about his mental health concerns. I had him engage in writing and some drawing assignments to attempt to pull out some of the underlying features of his anxious affect.
I administered the Rorschach. His responses were predictable. He had a large number of transparency and cross-sectional responses across the cards. Prominent in the cards were “dark shading responses” and the client’s focus on the black areas of the cards. This kind of response pattern represents anxiety which the client feels needs immediate alleviation.
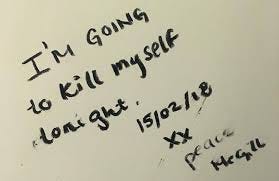
We slowly began to make progress when Craig brought a suicide note for me to read. In it, he described his overwhelming anxious state which he assumed got triggered from the stress of his first job, and now it was totally out of control. He wanted others to be free from him. He felt he was dragging the world downward.
When I showed the note to the psychiatrist, Craig was sent to the hospitalized again. The day before he was to check into the hospital, Craig disappeared. A few days later, they found his body inside of his car, Carbon Monoxide poisoning was ruled the cause of death.
In retrospect, it seemed his job situation triggered something already inside of Craig. Once set in motion, his thoughts moved quickly to suicide. He felt overwhelmed by a kind of lethal anxiety which rolled through him on a daily basis and it took everything he had to weather it. Even with all the help and support he was receiving, his mind was made up that nothing would dislodge this extreme emotional pain due to anxiety. He acted on his thoughts with suicide.
Could he have been stopped? Could he have been better protected? Was there a treatment that might have reached into his psyche and pulled him from his fateful course? No one will ever know. He left a trail of emotionally confused, discouraged, and beaten loved ones behind, but in his mind, suicide ultimately became the only course of action he thought that was available to him.
SUICIDE PREVENTION
Who hasn’t thought at one time or another about suicide. Maybe it is during a major life set-back or perhaps you have been rejected by a lover.
Suicide is such a common thought that there is a question in the Minnesota Multiphasic Personality Inventory (MMPI) about thoughts of dying that if not endorsed as true elevates the scale measuring response truthfulness.
The most important step for preventing suicide is to engage with the person who feels suicidal and attempt to bring out in the open the private thoughts around this lethal action that the person is holding. This is a list of the kinds of things that someone who is likely to act on suicide will start saying or doing.
Talking about suicide (making statements such as "I'm going to kill myself," "I wish I were dead" or "I wish I hadn't been born".
Getting the means to take one’s own life, such as buying a gun or stockpiling pills.
Withdrawing from social contact and wanting to be left alone.
Describing or showing large mood swings, such as being emotionally high one day and deeply discouraged the next.
Being preoccupied with death, dying or violence (such as in the news or on TV)
Feeling trapped or hopeless about a situation
Increasing use of alcohol or drugs
Changing normal routine, including eating or sleeping patterns. Poor sleep increases markedly the likelihood of acting impulsively.
Doing risky or self-destructive things such driving recklessly or cutting one’s arm or burning a finger.
Giving away belongings or getting affairs in order when there is no other logical explanation for doing this
Saying goodbye to people as if they won't be seen again
Showing gross personality changes such as saying that the person is severely anxious or agitated.
If you connect these to Craig’s case above, you will note that he was showing these signs.
Currently, the only way to ultimately prevent a suicide response is to restrain a person through hospital inpatient intervention, but this is challenging because it is not possible to put these restraints on for any appreciable length of time.
Suicide can be viewed as a larger social issue. This makes sense for prevention because it makes visible access to help and services that a person contemplating suicide may not be aware of.
Research has pointed to what are known as “modifiable” factors or protective features that are amenable to education and psychological intervention. These are listed below:
Access to means for suicide (guns)
Mental disorders (Generalized Anxiety Disorder)
Medical illnesses (treating medical conditions)
Social Isolation
Employment
Anxiety reduction
Hope
Improves life satisfaction
PERSONAL RISK FOR SUICIDAL IDEATION
This question underscores evaluating your own sense of vulnerability. One area of vulnerability is hope or hopelessness. In the 1990s I developed an instrument called “The Hoplessness Scale” (seeHill, R. D., Gallagher, D., Thompson, L. W., & Ishida, T. (1988). Hopelessness as a measure of suicidal intent in the depressed elderly. Psychology and Aging, 3(3), 230–232. https://doi.org/10.1037/0882-7974.3.3.230
Below are some of the questions: Respond to these on a True/False basis: (* are reverse scored). Scoring over 5 on this measure might indicate that you are vulnerable to feeling overwhelmed in a negative way about the future. Suicide is a strategy to stop the future from happening, so losing hope is a key for understanding why a person might contemplate suicide as an option.
I have hope when I think about my future.*
I often feel like giving up.
Bad things will always turn around.*
I can’t picture what the future will be like.
I feel like I can accomplish anything.*
I think I will do well for myself in the future.*
The future doesn’t look good.
I expect the best things will happen to me.*
Nothing goes right for me.
I am ready for the challenges that lie ahead*