I have SAD.
This sounds like a grammatically incorrect sentence, but if you know the acronym “SAD” the sentence makes sense.
SAD=Seasonal Affective Disorder
If you have SAD you will, at certain times of the year, feel sad, but Seasonal Affective Disorder is a lot more than just plain old sadness.
What is Seasonal Affective Disorder?
Let’s start with the word, “sad,” which in the dictionary is defined as: 1. affected by unhappiness or grief; sorrowful or mournful. A range of synonyms fit the state of being sad, including: unhappy, despondent, disconsolate, discouraged, gloomy, downcast, downhearted, depressed, dejected, melancholy
The definition of SAD is more elaborate.
First, SAD: is a “term” and not just a “word.” I use google.com here to get at a generally understood meaning of the TERM: SAD.
From google.com: (SAD) is a type of depression that's related to changes in seasons — SAD begins and ends at about the same time[s] every year. If you're like most people with SAD , your symptoms start in the fall and continue into the winter months, sapping your energy and making you feel moody.
This past week, a client asked, “Doctor, I’m certain I have SAD. Can you diagnose this for me?
I hedged a bit in telling this person that I couldn’t diagnose SAD, because, frankly, it is a hard condition to diagnose.
In fact, most diagnostic references do not consider SAD, in and of itself, a separate disorder, but rather, it is a sub-type of depression characterized by its recurrent seasonal pattern of symptoms lasting about 4 to 5 months per year. For this reason, the SAD symptoms are similar to major depression with the exception that the pattern of the disorder is impacted by the interaction of the external environment (Seasons) with the body. For example, specific SAD symptoms may differ for “winter-pattern” SAD than for “summer-pattern” SAD.
What Does SAD Look Like?
Again, this starts to get confusing because SAD is, in a way, time-sensitive depression. It is a kind of depression that has different seasonal symptom presentations in, say, the winter and in the summer. Most people who report SAD think that they have symptoms only in the winter, but the fact is, that they likely also experience symptoms in the summer, only the symptoms are different. Below is a listing that breaks this down:
Symptoms of major depression: Either with SAD or without SAD
Feeling depressed most of the day, nearly every day.
Losing interest in activities you once enjoyed.
Experiencing changes in appetite or weight.
Having problems with sleep.
Feeling sluggish or agitated.
Having low energy.
Feeling hopeless or worthless.
Having difficulty concentrating.
Having frequent thoughts of death or suicide.
Symptoms for winter-pattern SAD:
Oversleeping (hypersomnia).
Overeating, particularly with a craving for carbohydrates.
Weight gain.
Social withdrawal (feeling like “hibernating”).
Symptoms for summer-pattern SAD:
Trouble sleeping (insomnia).
Poor appetite, leading to weight loss.
Restlessness and agitation.
Anxiety.
Episodes of violent behavior.
How is SAD Diagnosed?
Diagnostic criteria for SAD vary across manuals, but for the DSM-5 and the ICD-10 there are common features that I’ve listed below:
The person must have symptoms of major depression.
Depressive episodes must occur during specific seasons (i.e., only during the winter months or the summer months) for at least 2 consecutive years. However, not all people with SAD experience symptoms every year.
The episodes of SAD (feel like hibernating) must be much more frequent than other depressive episodes in the season the person may be in (winter) versus other times of the year (during the year).
A client’s reported “Seasonal” pattern must be distinct and recognizable to the client.
Why is SAD Important?
SAD is important because it is prevalent. There is no strong epidemiological consensus around SAD, but it has been postulated that millions suffer from seasonal symptoms. Keep in mind that it is difficult to distinguish SAD from major depressive disorder.
It is thought that SAD occurs much more often in women than in men, and it is more common in those living farther north, where the daylight hours in winter are shorter. People in Alaska or New England likely develop SAD at a higher frequency than those living in Florida. SAD is acquired. It begins in young adulthood. People are not born with SAD, although they may be born with some genetic vulnerabilities towards it.
How Does SAD Operate?
People experience Seasonal Affective Disorder (SAD). Perhaps as important as acknowledging this is the research and clinical literature about how our human physiology and psyche are impacted by external forces like the seasons. With SAD, this is through our circadium rhythms. What are circadium rhythms? Circadian rhythms is the sleep-wake cycle which runs on a 24-hour pattern that is part of the body’s internal clock, operating mostly in the background.
Multiple theories describe how and why SAD operates.
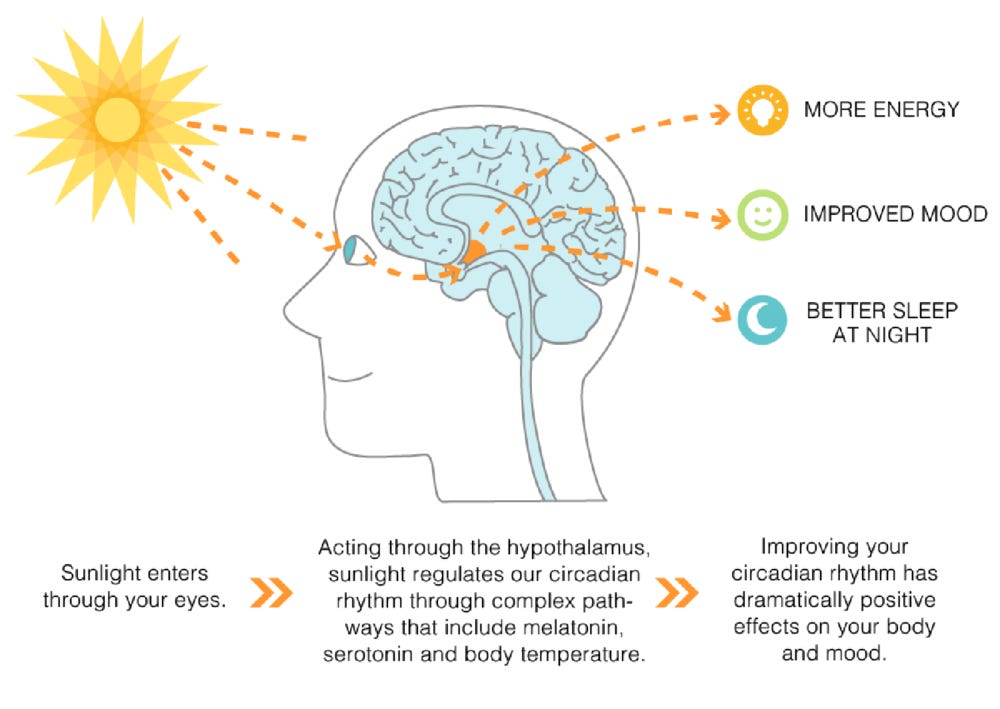
A feature of SAD that most people do understand is sunlight. From a population-demographic perspective, those persons living in regions where sunlight is prevalent experience fewer symptoms of SAD than those in regions where there are long periods of darkness. The figure above implies a direct connection between sunlight (as received through your eyes) and brain mechanisms associated with SAD. But, is the SAD issue that simple? More sunlight less SAD. For those who think so, treatments for SAD include the introduction of manufactured light to offset living in a dark region of the planet. Unfortunately, the issue of SAD is more complex than this diagram portrays.
There are several additional hypotheses used to investigate SAD and treatments for SAD. One is the Phase Shift Hypothesis (PSH). Briefly, the PSH hypothesis builds on the idea that SAD is due to a mismatch between the sleep/wake cycle and the circadian rhythms which are tied to the endogenous (or biological features within the individual). A key feature in the PSH hypothesis is the individual’s circadian pacemaker. The circadian pacemaker is a term that identifies nerve cells located in the hypothalamus that control 24-hour circadian rhythms and influence the sleep/wake cycle. The PSH hypothesis posits Phase-resetting agents (the addition of low-dose melatonin administration to bright light exposure for example). Such treatments phase-adjust the SAD patient’s circadian pacemaker, provided the treatment regimen is administered at the correct time.
Treatment Guided by the SAD PSH Hypothesis
The PSH hypothesis has been tested under a variety of settings. Below is a set of common guidelines for professionals who use the PSH hypothesis for treating SAD.
I’ve taken these guidelines from Lewy et al. Sleep Med Clin. 2009 Jun 1; 4(2): 285–299. Note: The level of light would be from a flouorescent light box that emits 10,000 lux light (lux is a measurement of light intensity).
If patients do not have early morning awakening, schedule 1–2 hours of 2500–10,000 lux exposure immediately upon awakening.
If patients begin treatment on the weekend, they may not have to arise earlier to accommodate the morning light exposure; early rising may retard the response for a few days.
The response begins 2 to 4 days after beginning light therapy and is usually complete within 2 weeks.
These patients should minimize any advance in their sleep time and should avoid bright light in the evening.
If patients do not respond to treatment, they may need a longer duration of morning light.
If patients respond only transiently or begin to complain of early morning awakening or severe fatigue in the evening, they may be becoming overly phase advanced due to too much morning light. The duration of morning light should be reduced but still begun immediately upon awakening or some late evening light exposure could be added.
Some patients may respond to an immediate “energizing” effect of bright light exposure (this may be a placebo effect), which if not administered too late in the evening might be helpful.
Once a response has been achieved, the duration and frequency of light exposures can be reduced. Always begin light exposure immediately upon awakening or a little later if patients become overly phase advanced.
If there is still no response, a trial of evening bright light (7–9 pm) may be necessary. These patients should minimize any delay in their sleep time and should avoid bright light in the morning.
Other Treatments for SAD
Treatments for mental health disorders, at least from modern medicine, general emerge from a psycho-environmental-biological model of some type. This is a highly reductionistic approach to treatment and very different than alternative medicine treatments which are based on wholistic models of human function that may or may not be reduced to concepts at, say, the cellular are molecular level. Accupuncture is a good example of the latter type of treatment
One model that has been used to guide treatment for SAD is the “photoperiodic” hypothesis. This hypothesis is built on similarities between symptoms of SAD and energy conserving strategies implemented by various animals that live at extreme northern latitudes. The strategic administration of melatonin emerges as a treatment from this line of thinking. Support for this comes from study after study demonstrating that patients with SAD have a longer duration of nocturnal melatonin secretion in winter than in the summer. In other words, SAD patients are predisposed to disruption in their natural melatonin secretions that should generally, in healthy persons, follow one’s circadium rhythms. In SAD patients, they do not.
The administration of melatonin is often combined with light therapy and a specific anti-depressant (Prozac - Fluoxetine). Timing of these drugs (and hormones) is often person-specific, so a period of monitoring a person’s sleep-wake cycle is usually conducted before treatment is administered. The idea here is to bring into focus and regularity, hormonal and neurotransmitter regulation.
Is this treatment effective?
It depends on how precisely and reliably the person is monitored, on the dosages administered, and on the follow-up that the patient receives. It is not an easy solution, but can produce substantial relief from SAD with the appropriate attention.